Background
CD47 is an innate immune checkpoint that binds signal regulatory protein alpha (SIRPα) and delivers a "do not eat" signal to suppress macrophage phagocytosis. Overexpression of CD47 serves as a mechanism of immune surveillance evasion, and is found to be associated with poor prognosis in both hematologic and solid malignancies. TTI-622 is a fusion protein consisting of the CD47-binding domain of human SIRPα linked to the Fc region of human IgG4. It is designed to enhance phagocytosis and antitumor activity by preventing CD47 from delivering its inhibitory signal as well as generating a moderate pro-phagocytic signal via IgG4 Fc. Importantly, unlike many CD47-blocking agents, TTI-622 does not bind to human red blood cells.
Methods
TTI-622-01 is an ongoing multicenter, Phase 1 study of the safety, tolerability, pharmacokinetics (PK), pharmacodynamics (PD), and preliminary antitumor activity of TTI-622 in adult patients with relapsed/refractory (R/R) lymphoma (NCT03530683). Based on a modified 3+3 scheme, weekly doses are escalated through pre-planned dose levels ranging from 0.05 to 8 mg/kg. The observation period for dose limiting toxicity (DLT) is the initial 3 weeks of treatment. Safety monitoring includes weekly clinical laboratories and assessments of adverse events (AEs) based on CTCAE v 4.03. Blood samples are collected for PK analysis and assessment of receptor occupancy on normal peripheral T cells. Disease assessments are performed per Lugano criteria every 8 weeks within the first 6 months, every 3 months up to two years, and every 6 months thereafter until the end of treatment.
Results
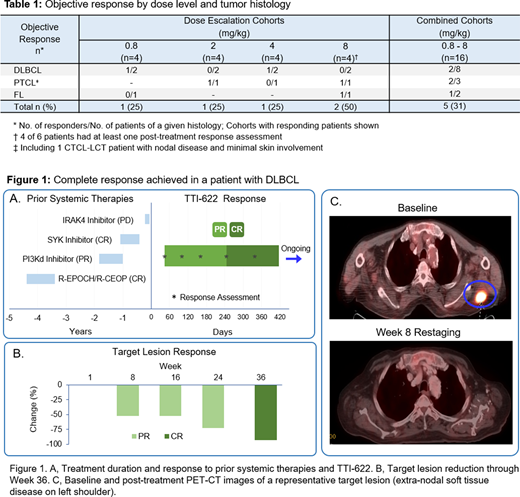
As of the July 16, 2020 cutoff, 25 patients (12M/13F) with a median age of 68 years (range 24-86) have received dose levels of 0.05−8 mg/kg with testing at 8 mg/kg ongoing. Patients with the following histologies have been enrolled: diffuse large B-cell lymphoma (DLBCL; n=13), Hodgkin lymphoma (n=5), follicular lymphoma (FL; n=2), peripheral T-cell lymphoma (PTCL; n=2), cutaneous T-cell lymphoma with CD30 negative large cell transformation (CTCL-LCT, n=2), and mantle cell lymphoma (n=1). Disease stages at entry have been III or IV in 23 patients; patients had received a median of 3 (range 1-9) prior systemic therapies including CAR-T in 5 patients and HSCT in 6 patients. Treatment-related AEs have been reported in 12 (48%) patients. Most AEs have been grade 1 or 2. The most frequent treatment-related AEs include thrombocytopenia (n=4; 1 grade ≥3), neutropenia (n=3; 3 grade ≥3) and fatigue (n=3; 0 grade ≥3). Grade 4 thrombocytopenia occurred in 1 patient in the 8 mg/kg cohort and accounted for the only DLT and treatment-related serious AE reported to date. This event that occurred on Day 8 was not associated with bleeding and resolved within 1 day after prophylactic platelet transfusion. Mild to moderate platelet decreases seen in the majority of patients generally occurred on dosing days and recovered quickly to baseline levels. No other grade ≥3 thrombocytopenia have been observed in the 4 other DLT evaluable patients dosed with 8 mg/kg to date. Preliminary PK results suggest dose-dependent increases in exposure following both single and repeated TTI-622 infusions. PD results indicate that end-of-infusion CD47 receptor occupancy (RO) is above 60% at doses ≥2 mg/kg and that RO is more sustained with TTI-622 doses ≥1 mg/kg compared to lower doses. Objective responses have been achieved in 5 patients, including 1 complete response (CR) in DLBCL (0.8 mg/kg) and 4 partial responses (PR) in PTCL (2 mg/kg), DLBCL (4 mg/kg), CTCL-LCT and FL (8 mg/kg). Initial responses were achieved at the first disease assessment (week 8) in all 5 responders including initial PR in the patient who subsequently achieved CR at week 36 (See Figure 1). In the dose range of 0.8-8 mg/kg, objective responses occurred in 31% (5/16) of patients with ≥1 post-treatment response assessment (See Table 1). Two of 4 response evaluable patients in the ongoing 8 mg/kg cohort achieved a PR, and 2 other patients have been on treatment for <8 weeks.
Conclusions
Results to date from this ongoing Phase 1 study in patients with R/R lymphomas indicate that weekly doses of TTI-622 up to 4 mg/kg are well tolerated with dose-dependent increases in exposure and RO. TTI-622 has shown activity in R/R lymphoma with objective responses across a broad dose range (0.8-8 mg/kg) and in multiple histologies. The study is currently evaluating the 8 mg/kg dose level.
Patel:Pharmacyclics: Consultancy, Speakers Bureau; Adaptive Biotechnologies: Consultancy; Janssen: Consultancy, Speakers Bureau; Genentech: Consultancy, Speakers Bureau; Kite: Consultancy; Celgene/BMS: Consultancy, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Consultancy, Research Funding, Speakers Bureau; BeiGene: Consultancy. Ramchandren:Seattle Genetics, Sandoz-Novartis, Pharmacyclics/Janssen, Bristol-Myers Squibb: Consultancy; Merck, Seattle Genetics, Janssen, Genentech: Research Funding. Lesokhin:Juno: Consultancy, Honoraria; BMS: Consultancy, Honoraria, Research Funding; Genentech: Research Funding; Janssen: Research Funding; GenMab: Consultancy, Honoraria; Serametrix Inc.: Patents & Royalties; Takeda: Consultancy, Honoraria. von Keudell:Pharmacyclics: Research Funding; Genentech: Research Funding; Bayer: Research Funding. Cheson:Symbio: Membership on an entity's Board of Directors or advisory committees; Morphosys: Consultancy; GSK: Membership on an entity's Board of Directors or advisory committees; Jannsen: Consultancy; Pharmacyclics: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding; TG Therapeutics: Speakers Bureau; Karyopharm: Consultancy, Membership on an entity's Board of Directors or advisory committees; Trillium: Research Funding; Kite: Consultancy; Parexel: Consultancy. Zonder:Intellia, Amgen, Takeda, Janssen, Regeneron, Alnylam, Caelum, Oncopeptides: Consultancy; BMS, Celgene: Research Funding. Seymour:Seattle Genetics: Research Funding; Merck: Research Funding; Karyopharm: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen/Pharmacyclics: Membership on an entity's Board of Directors or advisory committees; Incyte: Research Funding; Genentech: Research Funding; Bristol-Myers Squibb: Research Funding. Catalano:Trillium Therapeutics Inc.: Current Employment. Lin:Trillium Therapeutics Inc.: Current Employment. Uger:Trillium Therapeutics Inc.: Current Employment. Petrova:Trillium Therapeutics Inc.: Current Employment. Roberge:Trillium Therapeutics Inc.: Current Employment. Shou:Trillium Therapeutics Inc.: Current Employment. Iyer:Target Oncology: Honoraria; Seattle Genetics, Inc.: Research Funding; Rhizen: Research Funding; CRISPR: Research Funding; Curio Biosciences: Honoraria; Trillium: Research Funding; Daiichi Sankyo: Consultancy; Legend Biotech: Consultancy; Spectrum: Research Funding; Merck: Research Funding; Afffimed: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.